How 3D printing enabled a life-saving surgery on a complex spinal sarcoma
Pre-operative planning is crucial to delivering successful surgery, thereby delivering optimum patient outcomes. The arrival of 3D printed anatomical models has revolutionized how surgeons obtain the critical insights that are needed before performing complex surgical procedures, leading to better outcomes for patients. With the help of Axial3D, Mr. Alistair Irwin was able to successfully remove a complex spinal sarcoma from a young patient.
The Case
For over five years, Irwin has been a Consultant Orthopedic Surgeon, practicing at the Royal Victoria Infirmary in Newcastle Upon Tyne, one of just four specialist spinal sarcoma centers in England. Irwin undertakes all aspects of adult spinal surgery including minimally invasive techniques, with a specialist interest in spinal tumors, including spinal sarcomas shown in the case below.
How the team assesses tumors
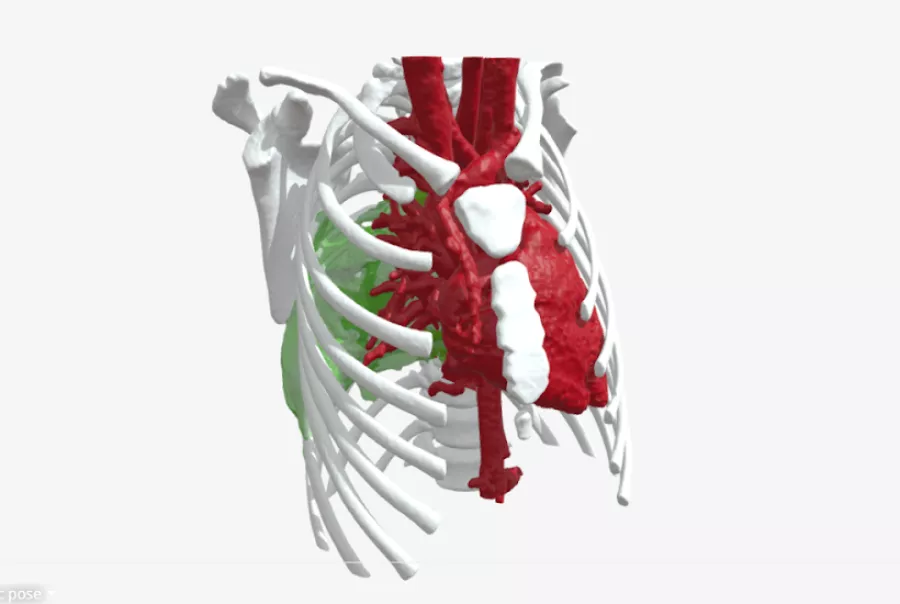
The team at Newcastle completes approximately 10 spinal sarcomas resections per year. In what is a one in a million case, a young girl from Newcastle UK was faced with an extremely rare and aggressive form of cancer that was growing quickly from the thoracic spine and chest wall into the anterior thoracic cavity and mediastinum. After biopsy this was diagnosed as a Mesenchymal Chondrosarcoma, a cartilage producing tumor that was rapidly destroying local structures and causing damage. If left alone, it could cause catastrophic harm - compressing vital structures (such as major veins, arteries and even the structure of the heart), or start to compress the spinal cord and cause damage to the nerves and motor functions. Complex spinal sarcomas are rare and require a highly specialized team including specialist oncologists, radiologists, pathologists and surgeons to care for them. In this particular case the site, size and complexity of the tumor required a surgical team comprising plastic, pediatric, cardiothoracic, pediatric cardiac and spinal surgeons. Because of its complexity, planning and visualization of the anatomical sites involved was crucial. This particular type of tumor is usually only treatable with radical surgery. However, because of the young age of the patient and aggressive nature of the tumor, a trial of adjuvant chemotherapy was started under the care of the pediatric oncologist. Unfortunately, the tumor continued to grow.
The Solution
This left two options for the team. Either declare the tumor inoperable because of its size and tricky location (sitting behind the heart, close to the lungs, bronchial tree, the aorta and the major Azygos vein in relation to the spine), or attempt to resect the tumor. This type of tumor must be removed in one procedure, as they are likely to grow back if they are removed in pieces. So, the only safe way to remove the tumor was in one single resection with a safe margin of healthy tissue surrounding it to ensure the entire tumor was successfully removed. The biggest difficulty for the team at this point was knowing exactly which structures were involved. Even with detailed MRI and CT imaging as well as transesophageal echo it was impossible for the team to ascertain whether the tumor was invading the heart or the atrium, or the involvement of the aorta and Azygos vein. To better assess the anatomy, one of the cardiothoracic surgeons had put a camera inside the patient’s chest to get a better look. However, due to the size of the tumor he was unable to get an accurate view of the anatomy and structures such as the heart or aorta. Attempting to resect the tumor without a complete understanding of it and the surrounding anatomy was far too great a risk.

Why the surgical team turned to 3D printing
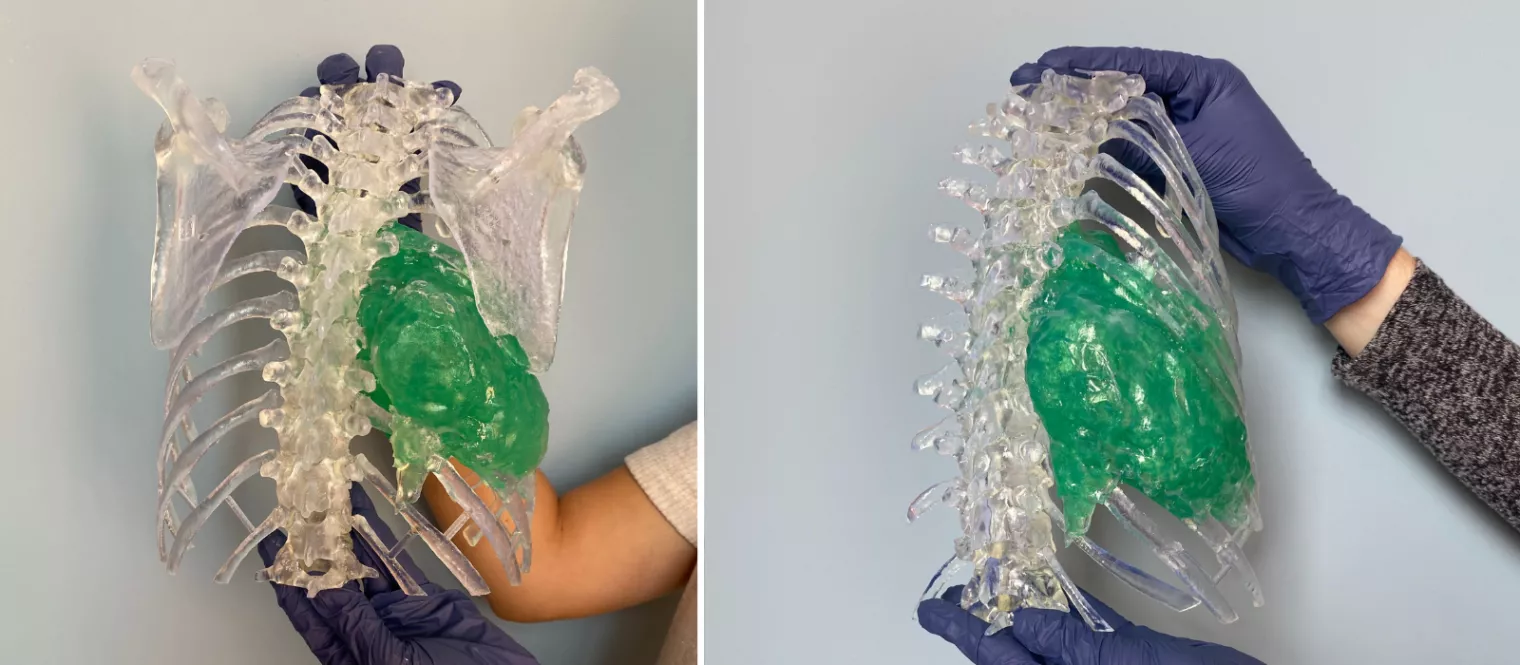
Being able to rely on Axial3D for these details and accurate models gave the surgical team a much clearer picture of the anatomy and enabled them to eliminate the guesswork well ahead of the resection.
The complex spinal sarcoma model became a critical tool in helping the team understand and plan exactly which ribs were intersecting with the tumor and how closely the team needed to make cuts on the ribs or the spine. Being able to practice on the model beforehand gave the team a great level of insightful detail on patient anatomy, and the confidence to carry out the procedure.
“It's easy to use, efficient, and quick. The models Axial3D produces are very good, accurate and easy to use. The service is fairly seamless and efficient compared to other types of new processes where it can be an onerous, complicated, lengthy process. The model produced in this case was very intuitive, very interactive and seamless which meant we could get things turned around quickly. I've been very impressed with how Axial3D can rapidly turn around complex requests,” Irwin said.
The outcomes for the patient have been incredibly positive. While she had to spend a few weeks in hospital after the procedure, she was able to walk out with no signs of weakness or paralysis. Her blood loss during the operation was at normal levels.
The greatest outcome of the model was the accurate tumor resection (confirmed by a pathology sample). After clear margins were determined and the young girl’s vitals were stable, she was able to return home with her family. With the help of the 3D printed model, she was discharged from the cancer ward with the comfort that the team had been able to resect the entirety of the tumor.
Disclaimer: Details of Axial3D's regulatory clearance for diagnostic use cases are outlined here. For all other uses of Axial3D solutions, they should be used for demonstration and education purposes only.
Experience 3D modeling in your own clinical practice. Trial Axial3D with a complimentary model for your next patient case.
Request a free anatomical visual